Glioblastoma, a highly aggressive form of brain cancer, presents significant challenges for patients and their families. Patients often experience a decline in neurological function and suffer from the harsh side effects of treatments, leading to a diminished quality of life and poor overall survival rates. While the benefits of integrating palliative care early in the oncology care pathway are well-documented, its utilization for glioblastoma patients remains notably low. This article explores the implementation and effectiveness of a Palliative Care Screening Tool designed to improve the identification and referral of glioblastoma patients to outpatient palliative care services. This quality improvement (QI) project investigated the feasibility, value, and effectiveness of adapting and using such a tool in a real-world clinical setting.
Glioblastoma, classified as a World Health Organization (WHO) grade IV glioma, is the most prevalent primary malignant tumor of the central nervous system. Despite advancements in treatment, the median survival for patients diagnosed with glioblastoma is only about 12 to 15 months. Throughout their illness, these individuals endure substantial neurological deterioration, resulting in a considerable burden for both patients and their caregivers. The need for palliative care in glioblastoma is particularly complex due to the multifaceted symptom burden arising from functional impairments, cognitive decline, and communication difficulties. Common symptoms include drowsiness, cognitive impairment, aphasia, motor weakness, seizures, and personality changes. Furthermore, treatments like chemotherapy and radiation therapy can induce additional distressing side effects such as nausea, vomiting, fatigue, and further cognitive decline.
Research indicates that despite the high symptom burden, patients with high-grade gliomas often receive less palliative care compared to those with other types of cancer. Several factors contribute to this underutilization. Patients and families may mistakenly believe palliative care is only appropriate at the very end of life. Healthcare providers may also equate palliative care with hospice, fearing it might diminish patient hope. Crucially, a lack of clarity among healthcare professionals regarding the criteria for palliative care referral may be a significant barrier.
A growing body of evidence supports the integration of early palliative care for patients with advanced cancer. Studies have demonstrated that early palliative care is associated with improved quality of life, reduced mood disturbances (like depression and anxiety), and even decreased healthcare costs. Despite this increasing recognition of the benefits, a significant gap remains in the understanding of how and when palliative care should be utilized, both among patients and healthcare providers. Lack of referral from healthcare providers is consistently identified as a primary obstacle to palliative care access. To address this referral gap, research suggests that employing a palliative care screening tool can effectively identify patients who would benefit from palliative care support and subsequently increase timely referrals. One study showed that using a screening tool significantly reduced the rate of missed palliative care referrals from 68% to just 16% within a four-month period.
Clinical practice guidelines from organizations like the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) recommend that outpatient oncology programs offer palliative care resources to cancer patients experiencing high physical and psychosocial symptom burden. The NCCN guidelines further advise repeated screening of all advanced cancer patients to determine the need for palliative care referral. However, reports indicate that the adoption of these guidelines into routine clinical practice is limited. Many institutions do not routinely screen oncology patients for palliative care needs, and uncertainty persists among healthcare providers regarding who should be referred and when. Therefore, the implementation of a standardized needs assessment, such as a palliative care screening tool, is essential to promote the role of palliative care in comprehensive oncology care. This quality improvement project aimed to address this gap by implementing a palliative care screening tool to increase the screening and referral rates for palliative care among glioblastoma (WHO grade IV) patients in an outpatient neuro-oncology clinic.
Objectives
This project was designed to evaluate the feasibility, value, and effectiveness of implementing a palliative care screening tool for glioblastoma (WHO grade IV) patients returning for follow-up evaluations at the Preston Robert Tisch Brain Tumor Center (PRTBTC) at Duke Cancer Institute (DCI).
The primary objectives were:
- Feasibility: To determine the proportion of eligible glioblastoma patients screened for palliative care needs using the glioma palliative care screening tool during routine outpatient visits.
- Value: To assess the proportion of patients who, based on their screening tool score (≥ 5), had a discussion about palliative care referral.
- Effectiveness: To evaluate the proportion of patients who were actually referred to palliative care among those who had a palliative care referral discussion.
Design and Methods
This quality improvement project utilized a prospective design to investigate the feasibility, value, and effectiveness of a palliative care screening tool in enhancing outpatient palliative care screening and referrals for glioblastoma patients. The project was deemed exempt from institutional review board review as it was classified as a QI initiative.
A comprehensive literature search was conducted to identify existing palliative care screening tools, specifically for neuro-oncology patients. While no tool was found specifically for this population, a simple palliative care screening tool developed for general outpatient oncology patients, based on NCCN palliative care screening criteria, was identified. This tool consists of five key screening items:
- Presence of metastatic or locally advanced cancer.
- Functional status score based on the Eastern Cooperative Oncology Group (ECOG) performance status.
- Presence of serious complications of advanced cancer associated with a prognosis of fewer than 12 months.
- Presence of serious comorbid diseases also associated with poor prognosis.
- Presence of palliative care problems.
A score of 5 or higher on this tool was recommended as a trigger for palliative care referral. This tool was adapted for glioblastoma patients in consultation with the neuro-oncology team at the PRTBTC. Adaptations included replacing “metastatic disease” with “progressive disease at current visit,” as glioblastoma is inherently an advanced disease within the central nervous system. The functional status scoring was adapted to incorporate Karnofsky Performance Status (KPS), the standard measure used at PRTBTC, alongside ECOG. Examples were added to clarify “serious complications” and “comorbid diseases.”
A provider questionnaire was developed to collect data including patient demographics, palliative care discussions, referral status, and reasons for not discussing or referring, if applicable. Prior to implementation, information sessions were held with clinical staff, including neuro-oncologists, advanced practice providers (APPs), nurse clinicians, and certified medical assistants (CMAs), to introduce the QI project and the palliative care screening tool.
During the 10-week project period, CMAs distributed the glioma palliative care screening tool and provider questionnaire to APPs for eligible patients. APPs performed palliative care needs screening during patient examinations, utilizing the tool and patient history. If the screening tool indicated a need for referral (score ≥ 5), the APP discussed palliative care referral with the attending physician and the patient. Referrals were made upon agreement from both the attending physician and the patient. Local patients were referred to Duke palliative medicine, while for out-of-state patients, recommendations for palliative care referral to their local oncologist were made. APPs then completed the questionnaire.
Setting and Participants
The project was conducted at the PRTBTC, a tertiary outpatient neuro-oncology clinic at the DCI in Durham, North Carolina. The clinic specializes in treating adult primary brain and spinal tumor patients.
Eligible patients were adults (≥ 18 years) diagnosed with WHO grade IV malignant glioma (glioblastoma or gliosarcoma), English-speaking, and returning to the PRTBTC for routine follow-up with a new brain MRI. Patients visiting for initial evaluations, new diagnoses, or those already receiving palliative care were excluded.
Key providers involved were 10 board-certified APPs (nurse practitioners and physician assistants), along with physicians, fellows, residents, and medical students.
Measurements
The project’s primary endpoint was the proportion of eligible patients screened for palliative care needs using the adapted palliative care screening tool. Secondary endpoints included the proportion of screened patients who scored ≥ 5 and had a palliative care discussion, and the proportion of patients referred to palliative care among those who had a discussion. Data were collected using the provider questionnaire and analyzed descriptively.
Results
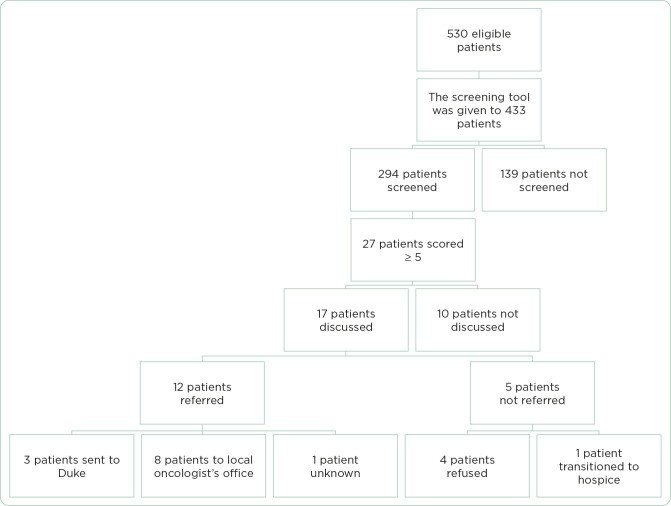
Over the 10-week implementation period, 530 patients were identified as eligible for screening. The palliative care screening tool was provided to providers for 433 of these patients. During the initial 17 days, due to logistical issues, the tool was not distributed for 97 eligible patients. Consequently, among the 433 patients for whom the tool was available, 294 (68%) were screened using the tool (Table 1). Overall, 56% (294/530) of all eligible patients were screened.
Figure 1.
Palliative care referral outcomes.
Table 1. Project Outcomes.
| Outcome | Estimate | 95% confidence interval |
|---|---|---|
| Proportion of eligible patients screened | 294/530 (56%) | 51%–60% |
| Proportion of eligible patients screened among those for whom the certified medical assistant provided the form to the APP | 294/433 (68%) | 64%–72% |
| Proportion of screened patients with score ≥ 5 | 27/294 (9%) | 5.9%–12.5% |
| Proportion of patients with score ≥ 5 who had a palliative care discussion | 17/27 (63%) | 42%–81% |
| Proportion of patients with score ≥ 5 who were referred to a palliative care consult | 12/27 (44%) | 25%–65% |
| Proportion of patients with referral among those with a palliative care discussion | 12/17 (71%) | 44%–90% |
The screened patient population was predominantly male (60%) and had a Karnofsky Performance Status (KPS) of 70% or higher (47%). Nearly half of the screened patients (45%) had a zero score on the NCCN Distress Thermometer. The majority (53%) were between 46 and 65 years of age (Table 2).
Table 2. Patient Demographics.
| Gender | |
|---|---|
| Male | 177 (60%) |
| Female | 109 (37%) |
| Unknown | 8 (3%) |
| Age | |
| < 25 | 18 (6%) |
| 26–35 | 39 (13%) |
| 36–45 | 49 (17%) |
| 46–55 | 84 (29%) |
| 56–65 | 71 (24%) |
| 66–75 | 21 (7%) |
| > 75 | 10 (4%) |
| Unknown | 2 (1%) |
| Karnofsky Performance Status | |
| 90%–100% | 133 (45%) |
| 70%–80% | 123 (42%) |
| 50%–60% | 35 (12%) |
| 30%–40% | 3 (1%) |
| 10%–20% | 0 (0%) |
| NCCN Distress Thermometer score | |
| 0 | 131 (45%) |
| 1 | 35 (12%) |
| 2 | 26 (9%) |
| 3 | 21 (7%) |
| 4 | 17 (6%) |
| 5 | 19 (6%) |
| 6 | 8 (3%) |
| 7 | 8 (3%) |
| 8 | 4 (1%) |
| 9 | 2 (1%) |
| 10 | 3 (1%) |
| Unknown | 20 (7%) |
Regarding feasibility (Aim 1), 56% of eligible patients were screened for palliative care needs using the glioma palliative care screening tool.
In assessing the value of the palliative care screening tool (Aim 2), 27 of 294 screened patients (9%) scored ≥ 5, indicating potential palliative care needs. Among these 27 patients, 63% (17/27) had a palliative care discussion. Reasons for not discussing palliative care for the remaining 10 patients included focusing on future treatment plans (5 patients), attending physician disagreement (3 patients), and unspecified reasons (2 patients).
For effectiveness (Aim 3), among the 17 patients who had a palliative care discussion, 71% (12/17) were referred to palliative care. Of these 12 referrals, 3 were to Duke palliative care, 8 were recommendations to local oncologist offices, and 1 lacked specific documentation. Among the 5 patients not referred, 4 refused referral, and 1 was referred to hospice.
The majority of screenings (89%) were conducted by APPs. Other providers involved in screening included fellows, residents, medical students, and one attending physician.
Discussion
Patients with high-grade gliomas, and particularly glioblastoma, face a substantial burden of neurological symptoms and treatment-related adverse effects. The benefits of early palliative care integration in oncology are well established. Given the unique and complex symptom burden in high-grade glioma patients, timely referral to palliative care is critical. This project highlights the importance of a palliative care screening tool in this context.
Historical data from the clinic showed an average of six brain tumor patients referred to Duke palliative care per 10-week period, and a pilot study of early palliative care integration had yielded approximately two referrals per 10 weeks. In contrast, this QI project, using a palliative care screening tool, resulted in 12 palliative care referrals within the 10-week period, with over half (56%) of eligible patients being screened. This demonstrates that integrating a palliative care screening tool into routine outpatient neuro-oncology care is feasible, raises awareness of palliative care needs, and significantly increases referrals.
Initial challenges with tool distribution by CMAs, affecting 18% of eligible patients in the first phase, were addressed by involving APPs and clinical staff in distribution. Integrating the palliative care screening tool into the electronic medical record system could further improve accessibility and ensure consistent utilization. Automated alerts based on screening scores could also promote long-term implementation and adherence.
The project’s multidisciplinary approach, particularly the active role of APPs, was crucial. APPs conducted the majority of screenings and initiated palliative care discussions, demonstrating their pivotal role in integrating palliative care into standard oncology practice.
While an extensive search did not identify a validated palliative care screening tool specifically for high-grade glioma patients, the adapted tool, based on a validated tool for general outpatient oncology patients, proved effective. The adaptation was carefully done in consultation with neuro-oncology experts at the PRTBTC, ensuring its relevance to this specific patient population. However, the lack of formal validation for this glioma-adapted palliative care screening tool is a limitation.
Despite identifying 27 patients as potentially needing palliative care based on the screening tool, palliative care discussions did not occur for 10 of them. Providers cited time constraints due to busy clinics and prioritization of treatment planning as reasons. Integrating palliative care visits with oncology visits could potentially address this barrier and facilitate better integration.
Furthermore, even when referral was recommended, four patients refused palliative care. This could be due to misunderstandings about palliative care (confusing it with hospice), time constraints, or financial concerns. Future research should explore patient perceptions and acceptance of palliative care referrals to optimize integration models.
Conclusion
This quality improvement project successfully demonstrated the feasibility of integrating a palliative care screening tool into routine outpatient neuro-oncology clinical care. The application of the palliative care screening tool effectively highlighted palliative care needs and led to a significant increase in palliative care referrals for glioblastoma patients. Enhancing accessibility of the tool, potentially through electronic medical record integration and automated alerts, could further improve its utilization. Addressing provider awareness of palliative care and patient acceptance of referrals are also crucial steps to ensure comprehensive screening and timely referrals. Ultimately, the use of a palliative care screening tool has the potential to facilitate earlier palliative care involvement, leading to improved symptom management and enhanced quality of life for patients with glioblastoma.
Appendix A. Glioma Palliative Care Screening Tool
| Screening items | Points | Patient points |
|---|---|---|
| Progressive MRI at current visit | 2 | |
| Functional status of patient (ECOG score/KPS score) | 0–4 | |
| 0: ECOG 0 = KPS 90%–100% | ||
| 1: ECOG 1 = KPS 70%–80% | ||
| 2: ECOG 2 = KPS 50%–60% | ||
| 3: ECOG 3 = KPS 30%–40% | ||
| 4: ECOG 4 = KPS 10%–20% | ||
| Any serious complication of cancer associated with a prognosis of < 12 months (e.g., metastatic disease to the spine, progression of disease more than twice, or new multifocal disease) | 1 | |
| Presence of one or more serious comorbid disease associated with poor prognosis (e.g., moderate-to-severe CHF, stroke, cognitive deficit, renal disease, liver disease, PE, bowel perforation, cerebral edema, obstructive hydrocephalus, cytopenia or NEW active problem requiring intervention or admission) | 1 | |
| Presence of palliative care problem | 1 | |
| • Uncontrolled symptoms (e.g., GI symptoms, headaches, fatigue, rash) | 1 | |
| • Moderate-to-severe distress (NCCN Distress Thermometer score of 4 or higher) | 1 | |
| • Patient/family concerns regarding course of disease and decision making | 1 | |
| • Patient/family requests palliative care consult | 1 | |
| • Team needs assistance with decision making | ||
| Total | 0–13 | |
| Refer the patient to palliative care when the score ≥ 5 | ||
| If the screening tool is not used, please write the reason below __________________________________________________________________________________________________ |
Note. ECOG = Eastern Cooperative Oncology Group; KPS = Karnofsky Performance Status; CHF = congestive heart failure; PE = pulmonary embolism; GI = gastrointestinal; NCCN = National Comprehensive Cancer Network. Adapted from Glare et al. (2011).
Appendix B. Provider Questionnaire
| Day # | __________ |
|---|---|
| Age | __________ |
| Diagnosis | __________________________________ |
| Sex | M/F |
| NCCN Distress score | __________ |
| Are you an APP? | □ Yes □ No: Fellow/Resident/Med student |
| Screening score ≥ 5? | |
| □ Yes □ No | |
| Palliative care discussion with the patient done? | |
| □ Yes □ No | |
| Referral made? | |
| □ Yes □ No | |
| If yes, referral made to | |
| □ Duke palliative care | |
| □ Recommended to patient’s local oncologist for palliative care referral | |
| If screening score ≥ 5, and discussion did NOT take place and/or referral NOT made, why? | |
| □ Patient refused | |
| □ Provider did not agree: Attending/APP (please circle one) | |
| □ Other: ___________________________________________________________________________________________ |
References
Footnotes
The authors have no conflicts of interest to disclose.